For Our Members
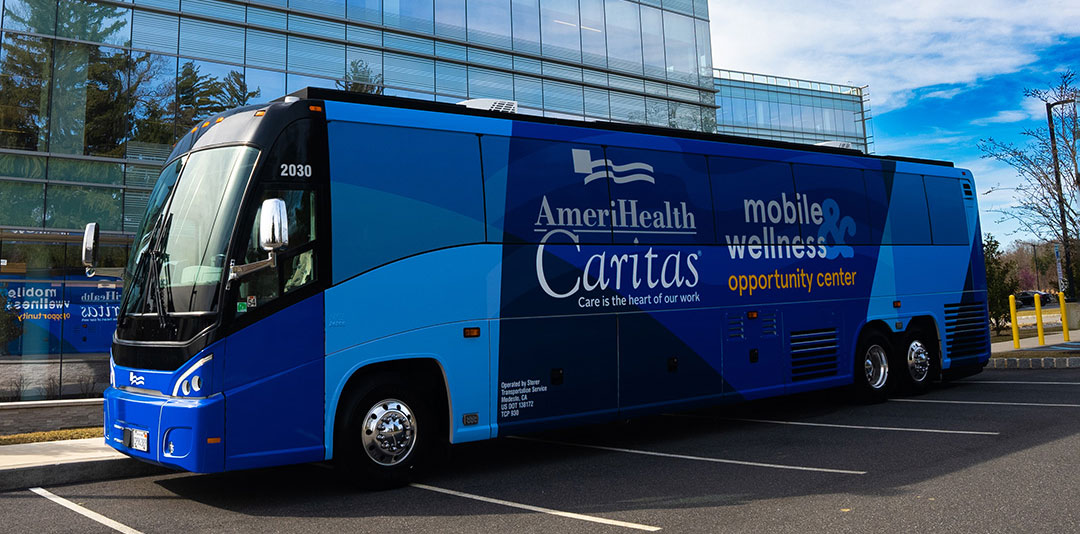
New! Mobile Wellness & Opportunity Center
Our state-of-the-art Mobile Wellness and Opportunity Center will provide community services in easy-to-access locations at no cost to members.
AmeriHealth Caritas Ohio would like to know what you think
Someone may be reaching out to you to answer a satisfaction survey about the health services you get from AmeriHealth Caritas Ohio. Your answers can help make sure you get the best care and service from us.
If you have any questions or want to know more about the survey, please call Member Services at 1-833-764-7700 (TTY 1-833-889-6446).
Share your Language Services feedback. Take the survey!
Comparta sus comentarios sobre los servicios de idiomas ¡Realice la encuesta!
Ban nou opinyon w sou sèvis nou bay nan lang pa w. Patisipe nan sondaj la!
AmeriHealth Caritas Ohio is now serving members statewide.
Your benefits*
Ohio Medicaid members can expect high-quality care through our:
- Large network of doctors and hospitals
- Caregiver programs for education and supports
- Disease management programs to help you stay healthy
AmeriHealth Caritas Ohio is unique because of our focus on whole-person care. We connect eligible members to services, such as:
- Mission GED: Adult members can get coaching and vouchers to take a high school equivalency exam at no cost.
- WW* (formerly Weight Watchers) online membership: Members ages 18 – 64 can get a WW membership at no cost for six months.
- CARE Card: Do things that help you stay healthy. Earn rewards on a reloadable gift card.
- Continuous glucose monitoring for members with diabetes: AmeriHealth Caritas Ohio is contracted with Pulsewrx to provide members living with diabetes with mobile smartphones. Apps and tools on the phone will support continuous glucose monitoring (CGM) so members with diabetes can have easier control of their blood sugar levels.
- Living Beyond Pain: This pain management program offers alternative treatment options.
- Food as Medicine: Qualifying members recently discharged from a hospital or enrolled in our diabetes program, and pregnant and post-delivery members and families can receive home-delivered meals at no cost.
- Vision care: Members ages 21 – 59 diagnosed with diabetes can get one additional eye exam every 12 months. This is in addition to the standard Medicaid benefit.
- Dental care: Members 21 and older can get one additional cleaning and exam per calendar year. Some restrictions and limitations apply. This is in addition to the standard Medicaid benefit.
- Transportation benefit: All members can get unlimited nonemergency trips for provider visits more than 30 miles from their home. Qualifying members can get up to 60 nonemergency one-way trips per year within 30 miles of their home, including unlimited additional trips for chemotherapy, radiation, dialysis, or prenatal and postpartum appointments and for medical services for members who use a wheelchair.
- Bright Start® program for pregnant members: Members get access to our pregnancy care program to help schedule appointments and connect to community resources and additional programs. Qualified members may receive a Bright Start Beginnings Bundle, which provides essential items for a new baby, including items to support a safe sleep environment and postpartum support.
- Housing stability flex funding: Access to a housing coordinator to identify local resources for safe and stable housing and up to $750 toward housing-related expenses in emergency situations for pregnant members.
- School uniforms: Up to $75 per child for school uniforms and school supplies. Contact your Care Guide for information on how to access these funds.
Have questions?
If you have questions about AmeriHealth Caritas Ohio, call Member Services at 1-833-764-7700 (TTY 1-833-889-6446), 24 hours a day, seven days a week.
If you are unsure if you are eligible to receive Medicaid or need to apply to receive Medicaid, resources are below:
- If you would like to apply to receive Medicaid benefits, please visit the Ohio Department of Medicaid (ODM) website or call 1-800-324-8680 (TTY 711).
- If you have questions regarding your eligibility for Medicaid, please visit ODM’s eligibility webpage.
- If you have questions relating to the Ohio Medicaid program, please call the ODM Contact Center at 1-800-324-8680 (TTY 711).
* These benefits will be available during the program year. Members receiving benefits must meet eligibility requirements.
If you have a problem reading or understanding this information or any other AmeriHealth Caritas Ohio information, please contact our Member Services toll-free at 1-833-764-7700 (TTY 1-833-889-6446), 24 hours a day, seven days a week, for help. We can explain this information, in English or in your primary language. You can get this document for free in other formats, such as different languages, large print, braille, or audio. Call toll-free 1-833-764-7700 (TTY 1-833-889-6446).
